So, you’re dealing with a dental abscess or infection and you’re not quite sure what to expect. Don’t worry, you’re not alone. In this article, we’ll take a closer look at the process for handling these dental issues, giving you the information you need to understand the steps involved in treating and resolving a dental abscess or infection. From diagnosing the problem to implementing the most appropriate treatment, we’ll cover it all. So, let’s dive in and get a better understanding of how to handle a dental abscess or infection.
Diagnosis of Dental Abscess or Infection
Performing a Physical Examination
When you visit the dentist with symptoms of a dental abscess or infection, the first step in the diagnosis process is a physical examination. The dentist will visually inspect your mouth and jaw area, looking for signs of swelling, redness, or an abnormal appearance of your gums or tooth. They may gently press on different areas to check for tenderness or pain, which can indicate the presence and location of the infection.
Gathering Medical History
In addition to the physical examination, your dentist will also gather your medical history to get a better understanding of your overall health and any pre-existing conditions that may contribute to the development of a dental abscess or infection. They may ask about your oral hygiene habits, previous dental procedures, and any medications you are currently taking. This information will help the dentist determine the cause of the infection and choose the most appropriate treatment.
Conducting Dental X-rays
Dental X-rays are an essential diagnostic tool when it comes to identifying dental abscesses or infections. These X-rays can reveal any abnormalities in your tooth structures, such as tooth decay, tooth fractures, or changes in the bone surrounding the tooth. X-rays can also help determine the extent of the infection and whether it has spread to the surrounding tissues or other teeth. By analyzing the X-rays, your dentist will be able to make an accurate diagnosis and plan the appropriate treatment.
Performing Other Diagnostic Tests
In some cases, your dentist may need to perform additional diagnostic tests to gather more information about the dental abscess or infection. This can include a dental pulp test, where the dentist checks the vitality of the tooth’s pulp by applying heat or cold to it. They may also take a sample of any discharge or fluid from the abscess for further analysis in a laboratory. These additional tests help confirm the diagnosis and ensure the most effective treatment plan is implemented.
Treatment of Dental Abscess or Infection
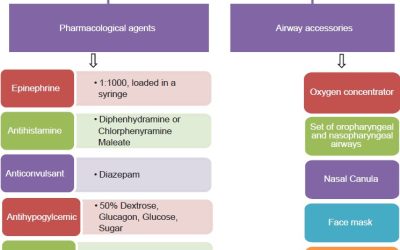
Prescribing Antibiotics
Once a diagnosis of a dental abscess or infection has been made, the next step is to start treatment. In most cases, antibiotics are prescribed to help fight the infection and prevent it from spreading further. The specific type and dosage of antibiotics will depend on the severity of the infection and your overall health condition. It is important to take the entire course of antibiotics as prescribed by your dentist to ensure the infection is completely eliminated.
Performing a Dental Drainage Procedure
In cases where the dental abscess has formed a pocket of pus, a dental drainage procedure may be necessary. This involves making a small incision in the abscess to drain the pus and relieve pressure. This procedure not only provides immediate relief from pain and swelling but also helps facilitate healing and allows the antibiotics to work more effectively. The dentist will ensure the area is properly cleaned and may place a dressing or drain to aid in the drainage process.
Performing a Root Canal Treatment
In situations where the dental abscess or infection has reached the innermost part of the tooth, the dental pulp, a root canal treatment may be required. This procedure involves removing the infected pulp, cleaning the root canals, and sealing them to prevent reinfection. By saving the tooth through root canal treatment, the natural tooth structure is preserved, and the risk of further complications is minimized. After the root canal, a dental crown is often placed on top for added protection and strength.
Extracting the Infected Tooth
In some cases, when the tooth is severely damaged or infected and cannot be saved through other treatments, extraction may be necessary. Extracting the infected tooth eliminates the source of the infection. After the extraction, your dentist will provide guidance on suitable tooth replacement options to restore both the function and appearance of your smile.
Monitoring and Follow-up
Post-treatment Instructions
Following the completion of any dental abscess or infection treatment, your dentist will provide you with post-treatment instructions. These instructions may include proper oral hygiene practices, such as brushing and flossing techniques, to maintain a clean and healthy mouth. You may also be advised to avoid certain foods or behaviors that could disrupt the healing process. It is essential to follow these instructions carefully for optimal recovery and to prevent any recurrence of the infection.
Prescribing Pain Medication
To manage any pain or discomfort during the healing process, your dentist may prescribe pain medication. These medications can help alleviate the pain associated with a dental abscess or infection, allowing you to feel more comfortable during your recovery. It is important to take the prescribed medication as directed and only for the recommended duration to prevent any potential side effects.
Scheduling Follow-up Appointments
After the initial treatment, your dentist will schedule follow-up appointments to monitor your progress and ensure that the infection is fully resolved. During these appointments, the dentist will conduct a thorough examination, including X-rays if necessary, to assess the healing of the affected area and check for any signs of recurrence. Regular follow-up appointments are crucial to catch any potential issues early on and to maintain optimal oral health.
Checking for Healing or Recurrence
During the follow-up appointments, your dentist will carefully evaluate the healing of the treated area and check for any signs of recurrence. They will examine the gums, tooth structures, and surrounding tissues to ensure that everything is healing properly. If any concerns are identified, further treatment or adjustments may be necessary. Regular monitoring is essential to ensure that the dental abscess or infection has been fully resolved and to prevent any complications.
Prevention of Dental Abscess or Infection
Maintaining Good Oral Hygiene
One of the most crucial aspects of preventing dental abscesses or infections is maintaining good oral hygiene. This includes brushing your teeth at least twice a day with a fluoride toothpaste, flossing daily to remove plaque and debris from between your teeth, and using an antibacterial mouthwash. By adopting proper oral hygiene practices, you can reduce the risk of tooth decay and gum disease, which are common underlying causes of dental abscesses and infections.
Regular Dental Check-ups and Cleanings
Regular dental check-ups and cleanings are essential for early detection and prevention of dental abscesses or infections. During these visits, your dentist will conduct a thorough examination of your teeth and gums, looking for any signs of potential problems or areas of concern. They will also perform professional dental cleanings to remove plaque and tartar buildup, which can contribute to the development of infections. By scheduling regular dental visits, you can address any dental issues promptly and prevent them from progressing into abscesses or infections.
Treating Dental Problems Promptly
It is important to address any dental problems promptly to prevent them from escalating into more severe conditions such as abscesses or infections. If you experience tooth decay, gum disease, or any other dental issues, seek dental treatment as soon as possible. Prompt intervention can help save your natural teeth, prevent further complications, and maintain optimal oral health.
Avoiding Risk Factors
There are certain risk factors that can increase the likelihood of developing dental abscesses or infections. These include poor oral hygiene, smoking, a weakened immune system, and a diet high in sugary or acidic foods. By avoiding these risk factors, you can significantly minimize the chances of developing a dental abscess or infection. Adopting a healthy lifestyle, following good oral hygiene practices, and making mindful dietary choices can go a long way in preventing dental issues.
Home Remedies for Dental Abscess or Infection
Rinsing with Warm Saltwater
One home remedy that can help alleviate the symptoms of a dental abscess or infection is rinsing your mouth with warm saltwater. Saltwater acts as a natural disinfectant and can help reduce swelling and pain. Mix half a teaspoon of salt in a glass of warm water and rinse your mouth thoroughly without swallowing. Repeat this several times a day to promote healing and relieve discomfort.
Applying a Cold Compress
To reduce swelling and minimize pain, applying a cold compress to the affected area can provide relief. Wrap a bag of ice or a cold pack in a thin cloth and apply it to the outside of your cheek where the abscess or infection is located. Hold it in place for 15-20 minutes and repeat as needed. The cold temperature helps numb the area and reduce inflammation, providing temporary comfort.
Using Over-the-counter Pain Relievers
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage the pain associated with a dental abscess or infection. Follow the instructions on the packaging and consult with your dentist or pharmacist if you have any concerns or specific medical conditions. It is important to note that these medications only provide temporary relief and should not replace dental treatment.
Avoiding Certain Foods and Beverages
While home remedies can offer some symptom relief, it is vital to avoid certain foods and beverages that can worsen the dental abscess or infection. Hard, sticky, or chewy foods can irritate the affected area and cause further discomfort. Additionally, avoid consuming sugary foods and beverages, as they can fuel the growth of bacteria and contribute to the progression of the infection. Stick to softer foods, such as soups, yogurt, and smoothies, until you receive professional dental treatment.
Signs and Symptoms of Dental Abscess or Infection
Severe Toothache
One of the hallmark symptoms of a dental abscess or infection is a severe toothache. The pain is often described as throbbing and persistent, and it may intensify when pressure is applied to the affected tooth. The pain can radiate to the surrounding areas, such as the jaw, ear, or neck. If you experience severe tooth pain, it is important to seek dental attention promptly to prevent further complications.
Swelling of the Face or Gums
Swelling of the face or gums is another common sign of a dental abscess or infection. The swelling can be localized to the area around the affected tooth or may involve a larger portion of the face depending on the severity of the infection. The gums may appear red, tender, or inflamed. If you notice any swelling or changes in your facial or gum appearance, it is crucial to seek immediate dental care.
Sensitivity to Temperature
If you have a dental abscess or infection, you may experience increased sensitivity to temperature changes in your mouth. This can manifest as pain or discomfort when consuming hot or cold food and beverages. The sensitivity is often localized to the affected tooth, but it can also affect nearby teeth and gums. Sensitivity to temperature should not be ignored, as it may indicate an underlying dental issue that requires professional attention.
Foul-smelling Breath
A foul-smelling breath, also known as halitosis, can be a telltale sign of a dental abscess or infection. The infection in the mouth releases unpleasant-smelling gases or substances, resulting in persistent bad breath. Even with regular oral hygiene practices, the foul odor may persist. If you have chronic bad breath accompanied by other symptoms, it is essential to consult with your dentist to determine the cause and appropriate treatment.
Complications of Untreated Dental Abscess or Infection
Spread of Infection to Other Areas
One of the most significant complications of an untreated dental abscess or infection is the spread of the infection to other areas of the body. The infection can travel through the bloodstream and potentially reach vital organs, such as the heart or brain. This can lead to serious health complications and even life-threatening conditions. Prompt treatment and proper management of dental abscesses or infections are crucial to prevent the infection from spreading.
Formation of Dental Fistulas
If a dental abscess or infection is left untreated, it may result in the formation of dental fistulas. Dental fistulas are abnormal channels or openings that develop between the infected tooth or gum and the skin of the face or mouth. These openings allow the pus to drain, relieving some of the pressure and pain associated with the abscess. However, dental fistulas are not a substitute for professional dental treatment and should not be ignored. Treatment of the underlying infection is still necessary to prevent further complications.
Bone and Tissue Damage
As a dental abscess or infection progresses, it can cause damage to the surrounding bone and tissues. The infection can erode the jawbone, leading to bone loss and weakening of the dental structures. If left untreated, this damage can make it more challenging to treat the infection and may require more extensive and invasive procedures to restore oral health. Timely intervention is crucial to avoid severe damage to the bone and tissues.
Systemic Infection
In rare cases, an untreated dental abscess or infection can lead to a systemic infection, which means the infection spreads throughout the body. This can result in serious health complications, including sepsis, a life-threatening condition characterized by widespread infection and organ dysfunction. Systemic infections require immediate medical attention, and early treatment of dental abscesses or infections is essential to prevent such complications.
Causes of Dental Abscess or Infection
Untreated Tooth Decay
One of the primary causes of dental abscesses or infections is untreated tooth decay. Tooth decay occurs when the protective enamel of the tooth is damaged, allowing bacteria to penetrate the deeper layers of the tooth. As the decay progresses, it can reach the pulp of the tooth, leading to infection and abscess formation. Regular dental care and addressing tooth decay promptly are important in preventing the development of dental abscesses or infections.
Gum Disease
Gum disease, also known as periodontal disease, is another common cause of dental abscesses or infections. When untreated, gum disease can cause the gums to become inflamed, leading to the formation of pockets between the gums and teeth. These pockets can become a breeding ground for bacteria, resulting in infections and abscesses. Maintaining good oral hygiene and seeking professional dental care for gum disease can help prevent associated complications.
Dental Trauma or Injury
Dental trauma or injury, such as a cracked tooth or a deep dental fracture, can also lead to the development of dental abscesses or infections. When the tooth structure is compromised, bacteria can enter the pulp or root canals, causing infection. It is important to seek immediate dental attention if you experience dental trauma or injury to prevent infections or abscesses from occurring.
Weakened Immune System
Having a weakened immune system puts you at a higher risk of developing dental abscesses or infections. Certain conditions, such as uncontrolled diabetes, HIV/AIDS, or undergoing cancer treatments, can weaken the immune system’s ability to fight off infections effectively. If you have a compromised immune system, it is crucial to prioritize oral health care and seek regular dental check-ups to catch any potential issues early on.
Types of Dental Abscess or Infection
Periapical Abscess
A periapical abscess is the most common type of dental abscess. It occurs when there is an infection at the tip of the tooth root, usually due to untreated tooth decay or a dental injury. The infection spreads from the tooth’s pulp to the surrounding tissues, leading to the formation of an abscess. Symptoms may include severe toothache, swelling, and sensitivity to temperature.
Periodontal Abscess
A periodontal abscess, also known as a gum abscess, occurs when there is an infection in the gums, typically resulting from untreated gum disease. The infection leads to the buildup of pus in the gum tissues, causing inflammation, pain, and swelling. Periodontal abscesses often occur in the space between the tooth and gum, known as the periodontal pocket.
Gingival Abscess
A gingival abscess is a localized infection in the gum tissue, usually caused by foreign objects, such as food particles or debris, becoming trapped between the tooth and gum. It can also occur due to gum trauma or injury. Symptoms may include a painful, swollen bump on the gum surface, tenderness, and discomfort. Gingival abscesses are typically less severe than other types of dental abscesses but still require prompt attention.
Pericoronal Abscess
A pericoronal abscess occurs when there is an infection around a partially erupted wisdom tooth. The wisdom tooth, or third molar, may not fully emerge from the gums, creating a flap of gum tissue known as an operculum. Bacteria and food particles can become trapped under the operculum, leading to infection and the formation of an abscess. Symptoms may include pain, swelling, difficulty opening the mouth, and a bad taste or odor.
Differences Between Dental Abscess and Dental Infection
Location of the Infection
The primary difference between a dental abscess and a dental infection lies in the location of the infection. A dental abscess refers to the collection of pus that forms within the tooth or surrounding tissues, while a dental infection simply indicates the presence of bacteria or other microorganisms causing an inflammatory response. Infection can occur in various parts of the tooth or mouth, while an abscess is a specific localized area where the infection has accumulated.
Severity of the Symptoms
The severity of the symptoms may also differ between a dental abscess and a dental infection. Dental abscesses typically exhibit more noticeable and intense symptoms, such as severe toothache, swelling, and facial pain. On the other hand, a dental infection may present with milder symptoms, such as sensitivity to temperature, minor discomfort, or mild gum inflammation. However, it is essential to remember that even mild symptoms should not be ignored, as they can progress into more severe conditions.
Affected Tooth Structures
In terms of affected tooth structures, a dental abscess typically involves the pulp and root of the tooth, resulting in an infection that can spread to the surrounding tissues. In contrast, a dental infection can occur within any part of the tooth, including the enamel, dentin, or even the gums. The specific location and extent of the infection can influence the appropriate treatment approach.
Treatment Approaches
The treatment approaches for a dental abscess and a dental infection can also vary. A dental abscess often requires immediate intervention, such as drainage of the abscess, root canal treatment, or tooth extraction. In contrast, a dental infection may be managed with antibiotics or other conservative measures, depending on the severity and cause of the infection. The treatment approach will be determined by the dentist based on factors such as the location, extent, and underlying cause of the infection.
In conclusion, the process for handling a dental abscess or infection involves a comprehensive diagnosis, proper treatment, careful monitoring, and preventive measures. It is essential to seek professional dental care if you experience any signs or symptoms of a dental abscess or infection to prevent complications and maintain optimal oral health. Remember to prioritize regular dental check-ups, maintain good oral hygiene practices, and promptly address any dental issues to minimize the risk of developing dental infections or abscesses.